Frequently Asked Questions and Answers
The effect of rheumatoid arthritis varies from person to person and requires a series of specialized diagnostic tests to be identified. Rheumatologists are specialized in diagnosing and treating more than 100 types of arthritic diseases, including rheumatoid arthritis. They often work with family doctors/GPs as consultants to advice and share their expertise regarding diagnosis and treatment of these diseases.
A detailed history plays a critical role in determining the nature of your symptoms. Be prepared to fill your detailed past medical history. Write down the list of questions you would like answered before your appointment is over. For example: How can I tell if my RA is progressing? What treatments should I know about? Keep in mind that the more you share with a rheumatologist about your condition, the better he or she will be able to diagnose and treat you.
During your first visit to the rheumatologist can be long visit in which the rheumatologist will listen to you describe your symptoms. Your rheumatologist may also perform a full musculoskeletal exam, which involves a focused examination of your joints and muscles. Rheumatologist may order a few necessary diagnostic tests as a part of work up to diagnose your disease. Once a diagnosis is made, your rheumatologist will explain the nature of your illness and what you might expect in the future. With an accurate diagnosis and a shared understanding of your illness, you and your rheumatologist can work together to design a treatment program aimed at managing pain and reducing inflammation to treat your disease.
Not true. People will not experience RA simply as a result of aging.
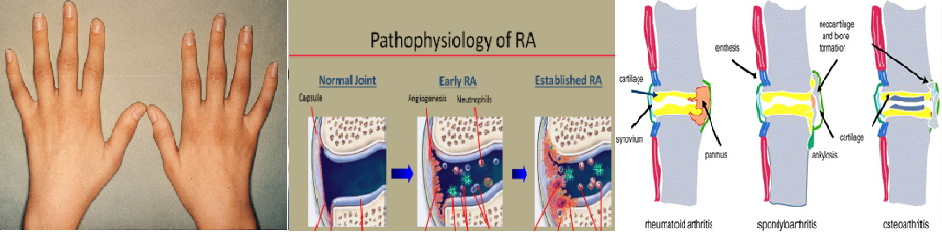
Osteoarthritis, on the other hand, is a very common "wear and tear" type of arthritis, and it has a very different presentation. Almost all of us experience this type of arthritis at one point or another. Commonly, you'll see it in the back (the spine), in the fingers, or in the thumb. This type of arthritis is not a systemic illness, like RA is. That means that it does not have effects outside of the joints. It's a local process. Osteoarthritis does not involve other organs the way RA does.
RA affects joints in a way that can alter the mechanics of the joints. Secondary osteoarthritis occurs due to altered stresses, in an attempt to repair the damage. Many people with RA may have to go for joint replacements often as a result of the secondary osteoarthritis.
People most commonly develop RA from the ages of 40-55, with an average age in the early 50s. About 1/3 of people with RA develop it after the age of 60.
Again, this is not true.
Some types of arthritis run in the family, but it is not like diabetes, where if both parents have it, the child will have it as well. We now know that even if you have genes that are associated with RA, you may not develop it. The genes are necessary, but not sufficient, to developing the disorder.
Something else has to happen - some kind of environmental trigger, like a virus, for example - for someone to develop RA. In some studies, for instance, smoking, along with a genetic predisposition, has been shown to increase the risk of RA.
Not true, one should definitely seek treatment.
In the present era many there are many treatment options with the help of which the affected person can lead productive life with minimum symptoms. The new biologic agents have profoundly altered the course and outcome of the illness. Early diagnosis of the disease is very important for best possible results.
It is very important to be under the care of a rheumatologist who understands the illness and is willing to, and does, participate in a partnership with your internist. The three of you have to form a very tight partnership with strong communication. Your outcome will be dependent not only on your RA, but the rest of your health.
Not at all, in many ways, the fatigue associated with RA can be worse than the pain.
Your friends and family members may not understand the nature of this fatigue. It is likely that in their experience, when they have a viral illness and they are in bed with aches, pains and fatigue, they can get up after a few days and return to normalcy.
The aches, pains and fatigue of RA do not resolve in the same way that is because the immunological inflammatory reaction of your RA has a bigger, chronic impact.
You can help those close to you understand by providing them with information about your RA so they can appreciate that you are not trying to avoid duties, responsibilities, or activities. They need to understand the nature of your RA, and "get it" just as you do.
Osteoarthritis is "just" a joint disorder, but RA can do much damage outside of the joints as well. It can affect internal organs. The inflammation in the joints can increase the risk of premature coronary artery disease or atherosclerosis, osteoporosis and it can even lead to an increased risk of lymphoma.
It is so important to control the inflammatory process of RA, because all of the aforementioned problems can be decreased or eliminated if the inflammation is controlled. Therein lies the importance of the interplay between you, your internist, and your rheumatologist.
Rheumatoid arthritis is a systemic disorder. It can affect the internal organs, although that is not as common as it was in the past. One of those tissues that can be inflamed is the eye, resulting in conditions such as scleritis.
It is well known that most internists treating a person with multiple chronic conditions may not focus on those problems that are less prominent. For this reason, it is very important to have a specialist who is designed to treat a particular disorder.
There are many new medications that can control the disease as well as systemic effects of the inflammation on other organs. Joint damage can be avoided, and those who are diagnosed and treated early on can, in particular, do quite well.
The efficacy of new medications is quite good. Some patients do well with traditional medications such as methotrexate and hydroxychloroquine . Newer medications like the anti-TNF biologic medications are also available and are more effective for a wide range of people. Higher cost is however limiting factor for the use of biologics in India.
Orthopedists are focused on the surgical repair of certain conditions, but their scope of practice in the treatment of rheumatic diseases is more limited in comparison with a rheumatologist.
Now that a number of effective yet highly complex new medications are available for RA, it is even more important that you see a rheumatologist for RA. Your internist or primary care physician can direct you to the proper musculoskeletal specialist for your particular issue, and, if necessary, can refer you to other specialists including physiatrists, radiologists, neurologists, or orthopedists.
Write to us
Have a Question? Simply send us a message. We'll give you the perfect answers.

